1. What to do when a tick bites you?
In the event of a tick bite, the tick should always be removed - and as soon as possible - in order to minimize the risk of transmission of pathogens. Antibiotic treatment, on the other hand, is only indicated if symptoms typical of Lyme disease (see symptoms) occur during the course of the disease [1, 2].
1.1. Removing the tick
It is important to remove the tick as completely as possible.The following technique is recommended [3, 4]:
- Take a small pair of tweezers to grasp the tick as close to the skin surface as possible. However, you should not squeeze the body of the tick [3, 4].
- Now you can pull the tick out carefully but firmly, applying even pressure. Avoid shaking or twisting the tick. This would increase the likelihood of the tick's mouthparts breaking off and remaining in the skin [3, 4].
- After removing the tick, disinfect the bite site and clean your hands with alcohol or soap and water [3, 4].
- If no tweezers are available, remove the tick by hand. It is best to use a piece of paper or cloth to protect your fingers when pulling it out [3].
- After removing the tick, the affected person should observe the bite site for 6 weeks for the development of erythema migrans (EM) (see symptoms) [3, 4].
1.1.1 What should you do if the head gets stuck?
If the tick's mouthparts remain in the skin when you pull it out, wait until they fall out by themselves. Further manipulation would only increase the risk of infection [3].
1.2. Home remedies
The use of household remedies is strongly discouraged when removing a tick. For example, the application of Vaseline, fingernail polish, isopropyl alcohol or a hot match has been shown to cause the tick's mouthparts to remain in the skin more frequently [3, 4].
In some countries, such as Australia, the freezing of ticks before removal is advocated. However, this is due to certain characteristics (toxin release) of the tick species native to these countries. In other regions, this is therefore not recommended [3].
1.3. Medication
In many cases, there are no symptoms after a tick bite.
In these cases, treatment with medication is not recommended—not even in the sense of prophylaxis [4]. The background to this is that in studies, prophylactic antibiotics had to be administered to 125 asymptomatic patients in order to prevent a single case of the disease. At the same time, however, there is a risk of adverse drug reactions and the development of resistance [4].
The effectiveness of antibiotic ointments is unclear and is therefore also not recommended [4].
1.4.Vaccination against TBE
In Europe, there are two main diseases that can be transmitted by ticks:Lyme disease and tick-borne encephalitis (TBE) [5, 6]. Although Lyme disease is more common, there is only a vaccination against TBE. This is recommended when traveling to corresponding risk areas—especially if you plan to spend time in nature [5, 6].
1.5 Tick risk areas
You can find a list of all relevant risk areas in Germany here.
2. When should you see a doctor when bitten by a tick?
In general, treatment after a tick bite only makes sense if symptoms occur during the course of the infection. Babies, children and pregnant women are not exempt from this [4, 7].
If you have difficulties in correctly classifying certain—possibly new—complaints, it is advisable to contact your treating physician in case of doubt.
2.1. Baby, child & pregnancy
For babies, children and pregnant women, the treatment—as with other groups of people— depends on the respective clinical picture (Lyme disease or TBE) and the corresponding symptom stage (see below) [8].
In the case of pregnant women, the treating physicians will also sometimes resort to other antibiotics, as these are better tolerated during pregnancy [8].
3. Symptoms of tick bites in humans
As already mentioned, there are two main diseases in Europe that can be transmitted by ticks: Lyme disease and tick-borne encephalitis (TBE) [5, 6].
The symptoms of both diseases differ significantly and are therefore treated separately below.
Symptoms of both Lyme disease and TBE can appear after just a few days or weeks. However, in the case of Lyme disease in particular, certain symptoms may not appear until much later—months or even years later [9, 10].
3.1. When do symptoms occur?
A previous tick bite or the skin changes typical of Lyme disease ("erythema migrans", see below), which are by no means always present, are not even remembered by many sufferers in retrospect [11].
3.2. Redness and red circle
Redness or a red circle are among the most common symptoms after a tick bite. As this symptom is typical for Lyme borreliosis, but not for tick-borne encephalitis (TBE), you can find more information on this in the following section under
4. Diseases caused by tick bites
4.1. Lyme disease
Lyme borreliosis is an infectious disease transmitted by ticks. However, the actual disease trigger is the so-called "Borrelia burgdorferi" bacteria. The ticks therefore only serve as a vector, a "vehicle" [5]. The probability of a tick bite is highest during the summer months. Exposure sites are tall grasses, bushes and wooded areas. However, ticks cannot jump. Direct contact is therefore necessary [5, 12].
4.1.1 The probability of contracting Lyme disease
The exact risk of infection always depends on the individual case. However, it depends on the following factors, some of which are difficult to assess for those affected [1, 13]:
- Whether the tick belongs to the so-called "Ixodes" species (in Europe, this would primarily be "Ixodes ricinus", also known as the "common wood tick")
- What stage of development the tick was in (larva, nymph, or adult—nymph stage with the highest risk of transmission)
- How long the tick was attached (rather low risk in the first 48 hours)
Even in endemic areas, not all ticks are infected with the Borrelia burgdorferi bacteria. In one study, for example, 15 % of all ticks were infected [13].
4.1.2 Symptoms of Lyme disease
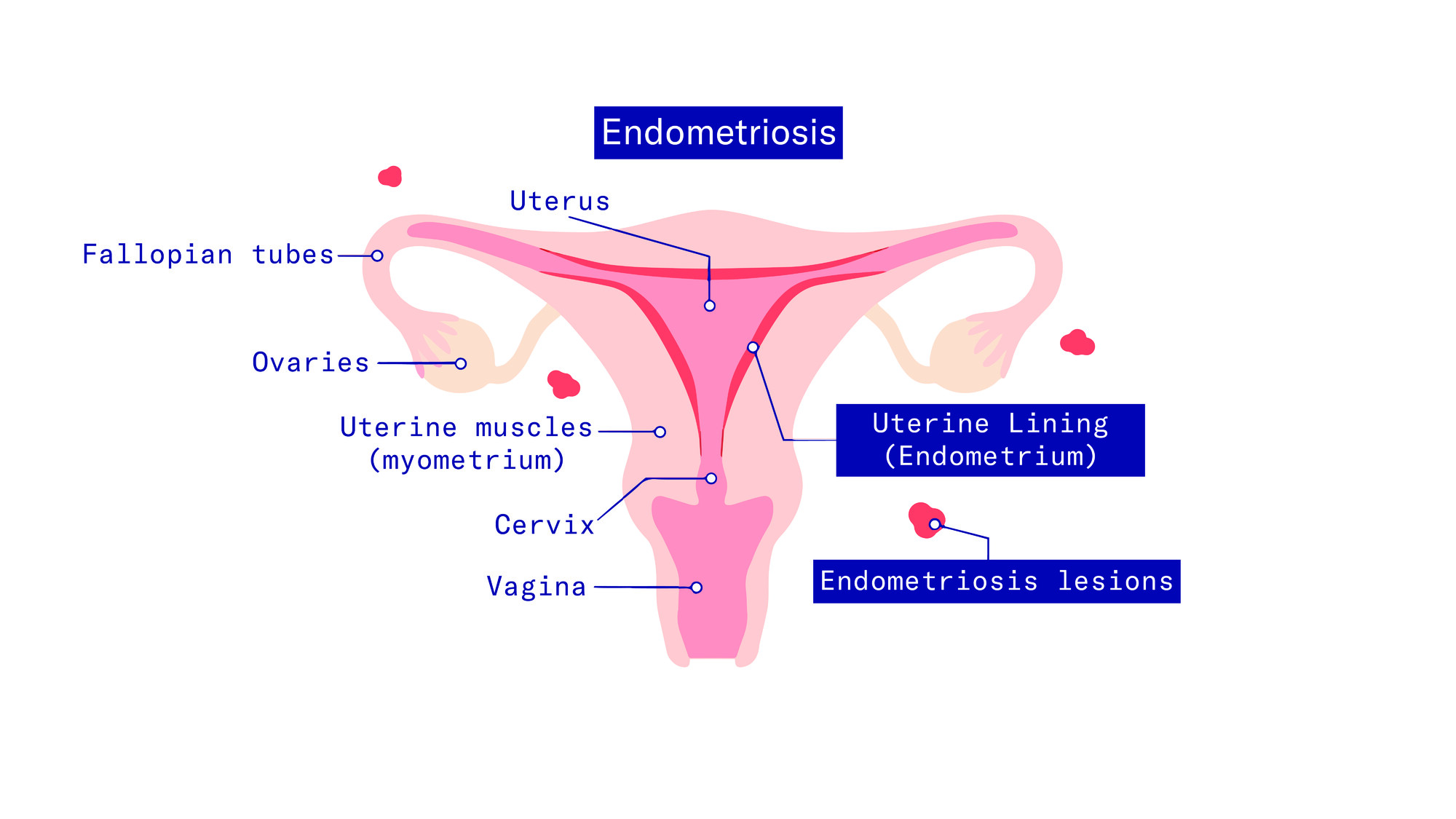
A Lyme disease infection usually manifests itself as redness that increases in size from the injection site. If left untreated, further symptoms such as nerve, heart, or joint involvement can occur later on [9, 14].
4.1.2.1 Redness & red circle (erythema migrans)
After a few days to weeks without any noticeable change in the skin, a circular, spreading, bright red skin change may appear from the bite site. Due to the spreading, the redness is also referred to as migratory erythema or "erythema migrans" in Latin [9, 14].
This symptom is the most common and typically the earliest symptom of Lyme borreliosis. Nevertheless, it only occurs in around 50 % of all infected people—so it is by no means a "must". In another 30 % of all people with erythema migrans, there is also a fading in the middle of the redness [9, 14].

4.1.2.2 Itching
Erythema migrans is often the only symptom of Lyme disease. While pain due to redness is rare, it can occasionally be accompanied by itching [9, 14].
4.1.2.3 Other Lyme disease symptoms
Much rarer, but also an "early Lyme disease symptom", is the so-called "lymphadenosis cutis benigna". This is an immunological reaction that leads to red-bluish skin nodules and locally swollen lymph nodes. The lumps usually affect the earlobes or nipples [9, 14].
The symptoms, which typically only appear after weeks to months, include so-called "acute neuroborreliosis" and "Lyme carditis" [9, 14].
The former is also known as "early neuroborreliosis" and influences 3 to 12 % of all Lyme disease sufferers. Symptoms are often nerve pain radiating from the spine, especially at night, sometimes intense, paralysis of the extremities and cranial nerve deficits [9, 14].
However, these symptoms usually resolve within several weeks with antibiotic treatment [9, 14].
Lyme carditis, on the other hand, affects around 4 % of all infected people and is an inflammation of the heart muscle, which in many cases remains asymptomatic. However, cardiac arrhythmia, shortness of breath and chest pain can also occur [9, 14].
4.1.3. Blood values for Lyme disease
Erythema migrans, i.e., the migratory redness typical of Lyme disease, is a so-called visual diagnosis. It is therefore sufficient for the treating physicians to see the appearance of the skin in order to initiate antibiotic treatment [11, 15].
However, this symptom only occurs in 50% of all infected people. And even among these, not everyone notices it. A laboratory blood test is therefore considered for all other symptoms typical of Lyme disease (see above). Without symptoms, however, no blood tests should be carried out [11, 15].
In the blood test, doctors then test for Borrelia-specific antibodies. Direct detection of the pathogen is extremely difficult in Lyme disease [11, 15].
4.1.4. Treatment of Lyme disease
Symptomatic Lyme disease should always be treated with antibiotics. In most cases, the preparation "Doxycycline" or "Amoxicillin" is used. However, the choice of antibiotic always depends on the current stage of the disease. Other preparations can therefore also be used [2, 16].
However, there is no benefit from a particularly high dose, a combination of different antibiotics or long-term therapy, which is why all of these are not recommended [2].
4.1.5 Late effects
There are a number of possible late effects that only appear months or years later. These include so-called "Lyme arthritis", "acrodermatitis chronica atrophicans" and "chronic neuroborreliosis". These can develop if Lyme disease remains untreated [9, 14].
While the former is an inflammation of the joints (usually large joints such as knees), the latter is a chronic skin change on the extensor sides of the extremities (usually lower legs). Chronic neuroborreliosis" is very rare. In this case, the inflammation spreads to the brain [9, 14].
4.1.6. Is Lyme Disease Contagious?
Scientific studies clearly demonstrate that Lyme disease is not transmissible from person to person. Individuals who are infected with the disease are therefore not contagious to their surroundings. Transmission occurs exclusively through ticks as vectors.[20]
4.2. TBE
Tick-borne encephalitis (TBE) is the second main tick-borne disease in Europe after Lyme disease. Here too, ticks are only vectors, i.e. "vehicles". However, in contrast to Lyme disease, the pathogen is a virus [5, 6].The TBE virus also infects ticks of the so-called "Ixodes" species.In Europe, this is "Ixodes ricinus", also known as the "common wood tick" [17].
4.2.1 Symptoms of tick-borne encephalitis
It usually takes between 7 and 28 days from infection to the onset of symptoms in TBE, with 90% of all infected people having an asymptomatic course anyway [10].
In the remaining 10 %, the disease usually has a two-phase course. Initially, flu-like symptoms such as fever or aching limbs occur and only then (after a fever-free interval) is there a further rise in temperature coupled with brain (skin) inflammation [10]. This can be accompanied by headaches, clouding of consciousness, vomiting or diarrhea, for example. In children, the course is on average milder [10].
4.2.2 Diagnosis and treatment of tick-borne encephalitis
TBE can be detected in a laboratory blood test. Depending on the phase of the disease, the pathogen is detected either directly or indirectly via antibodies [18].
Treatment is only symptomatic and aims to reduce the fever. However, people who spend a lot of time in risk areas or plan to travel there have the option of being vaccinated in advance as a preventative measure [7, 19].
A list of all relevant risk areas in Germany can be found here.
4.2.3. Vaccination Schedule for TBE
The TBE (Tick-Borne Encephalitis) vaccination provides a graduated protection buildup:
- First vaccination dose: No vaccine protection yet present
- Second vaccination dose: 82% protection rate for approximately 1 year
- Third vaccination dose: 97% protection rate for at least 3–5 years
The vaccine protection remains good even 5–10 years after the primary immunization series.
With an accelerated vaccination schedule, vaccine protection can also be established on short notice, for example before traveling to a risk area. Booster vaccinations are required after 3 or 5 years, depending on age. [20]
The contents of this article reflect the current scientific status at the time of publication and were written to the best of our knowledge. Nevertheless, the article does not replace medical advice and diagnosis. If you have any questions, consult your general practitioner.
Originally published on