1. Vaccination – the artificial stimulation of an antibody-mediated immune response
The coronavirus pandemic has turned the attention of the public to the subject of vaccination. What are the benefits and risks of vaccines? Who benefits most and for how long? How big are the differences between the various types of vaccines? In order to understand exactly what vaccination is, what types exist, and how vaccines work, it is useful to know the basics of the human immune system and what is known as acquired immunity. This is explained in detail in the first part of the Data4Life series of articles on immunity. Acquired immunity can be summed up as follows: When the body comes into contact with a disease-causing microbe (pathogen), the response to the pathogen is stored in the immunological memory in the form of tailored antibodies. When the body encounters the same pathogen a second time, the defense mechanisms responsible for antibody production are activated immediately.
A brief history of vaccination
Although there are reports of very simple forms of vaccination being used as early as the fifteenth century in China and India, the story of modern vaccinations is generally considered to begin with the work of Edward Jenner [1]. Virtually unknown among the general public, the English doctor and scientist is referred to by specialists as the “father of immunology.” His work in the eighteenth century focused on cowpox (Variolae vaccinae), from which the word “vaccine” is derived. Jenner’s research led to the development of a widely available vaccine against smallpox that saved countless lives [2]. Since these initial groundbreaking discoveries, the production of vaccines has undergone constant development and the resulting global vaccination programs are regarded as a revolution in healthcare.
Active and passive vaccination approaches
All vaccines work on the same basic principle: to prepare the body to fight a pathogen that it has not encountered before. This can be achieved through active or passive vaccination (immunization) [3].
Active immunization
Active immunization works by exposing the body to a weakened (attenuated) or inactivated pathogen, which stimulates the immune system to produce the necessary antibodies. When the body encounters the “real” pathogen again, specific antibodies are already available, as if the immunized person had been naturally infected in the past. This type of artificial active immunization, therefore, protects against a naturally occurring initial infection as well as its symptoms.
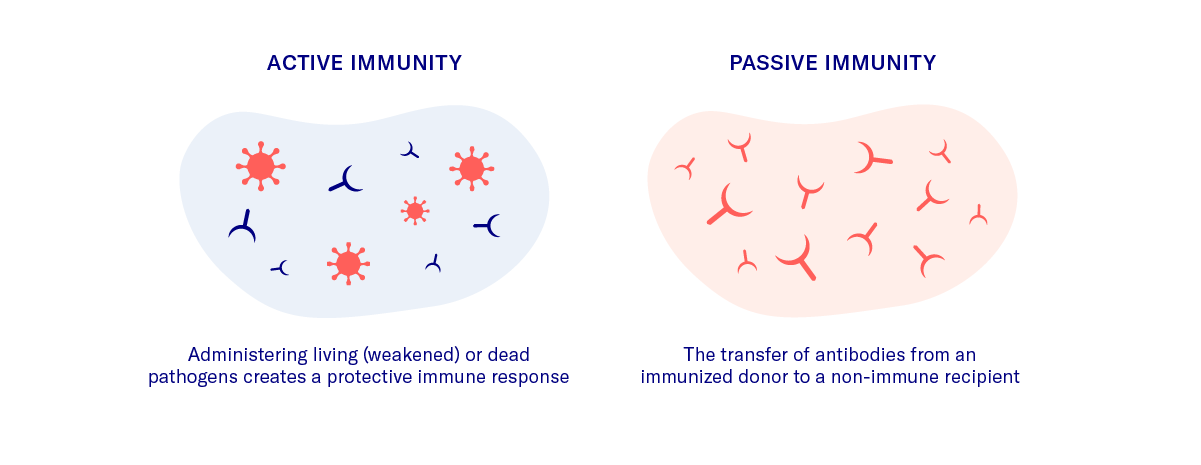
Passive immunization
Artificial passive immunization involves extracting antibodies against a specific pathogen from the blood of one person, processing the antibodies, and then administering them to another person. Natural passive immunization is acquired in a similar way. In this case, maternal antibodies cross the placenta to the fetus and later pass to the newborn through the breastmilk. The fetus or newborn does not produce its own antibodies but instead acquires passive immunity against disease from the mother. Antibodies acquired as a result of passive immunization decline over time, which means that the person receiving the antibodies is protected for a limited period only.
Nowadays, active immunization is the most commonly used form of vaccination. Unlike passive immunization, it stimulates the body to produce its own antibodies, which confers longer-lasting immunity.
Tetanus (lockjaw) vaccination is a well-known case in which both active and passive immunization approaches are regularly used. Antibody therapy was first used in 1890 to achieve passive immunization. This “antiserum” is still used today because it offers rapid and effective immunity, although this only lasts for a few weeks. For this reason, it is only used in acute cases, for example, for a heavily contaminated wound in a person whose immunization status is unknown. The preventive vaccine that is used worldwide nowadays is based on the active immunization developed in 1924. The immune response generated in the body is not directed at the pathogen itself but at the toxin produced by the pathogen, which is responsible for deadly tetanus infections [4].
Types of vaccines
Various types of vaccines exist that use pathogens in different states (for example, live or inactivated) or parts of a pathogen to stimulate the required immune response [5].
Live vaccines
Live vaccines use a live, but weakened (attenuated) form of the pathogen. This allows the pathogen to proliferate in the body and stimulate the necessary immune response (antibody production) quickly. Because the pathogen is still active, care must be taken when administering live vaccines to people with compromised immune systems.
Inactivated vaccines
Unlike live vaccines, inactivated vaccines are made from killed microorganisms or parts of microorganisms that are no longer able to proliferate. Consequently, the immune response is slower and less intense. Therefore, additional substances (adjuvants) are usually required to stimulate the necessary immune response and regular booster vaccinations are necessary. Inactivated vaccines have the advantage that unwanted side effects or symptoms are less common.
From a historical perspective, these are the two main types of vaccinations. However, many other types of vaccinations exist, which use, for example, the outer envelopes of pathogens, toxins produced by pathogens, or gene sequences of viruses to stimulate antibody production.
Vaccination and herd immunity
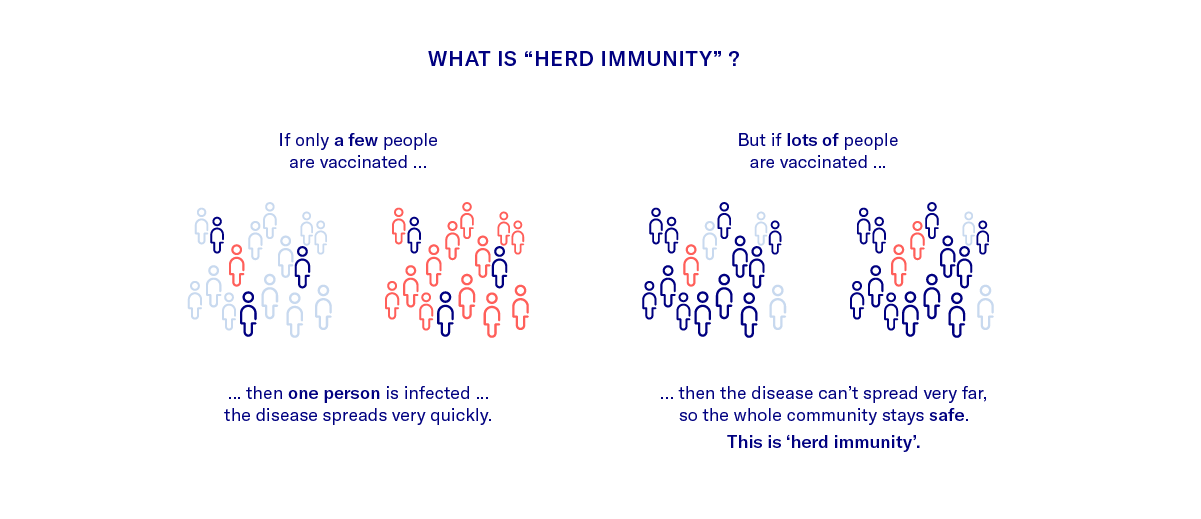
Herd immunity describes the phenomenon whereby (depending on the pathogen) not everyone in a population needs to be immune to prevent the spread of disease. If a sufficiently high percentage of the population is immune, the spread of the disease is stopped because there are not enough new non-immune hosts to infect. The few at-risk individuals are therefore protected because they are surrounded by immune members of the herd. The percentage of immune individuals necessary to disrupt transmission and achieve herd immunity depends to a large extent on the infectivity of the pathogen. The more infectious the pathogen, the greater the percentage of the overall population that needs to be immune (with a theoretical maximum value of 100%) [6]. Mass vaccination programs are based on the concept of herd immunity. Measles, mumps, polio, and smallpox are examples of diseases that were once very common but are now very rare in parts of the world – or have been completely eradicated – because large-scale vaccination programs helped to establish herd immunity without 100% of the population needing to be immune. Herd immunity can also be achieved if a large part of the population becomes immune to a disease by developing immunity after infection and recovery [7]. Local outbreaks of diseases such as measles are still seen in Germany, however, where the vaccination rate has for some time been just below the percentage that would be necessary for herd immunity.
2. Coronavirus (SARS-CoV-2) and immunity
But what about immunity in the context of coronavirus (SARS-CoV-2)? Studies indicate that infection results in the production of typical antibodies. The presence of these antibodies forms the basis for the antibody detection test, which is used to determine whether a person has been infected with the coronavirus. More information about coronavirus antibodies and the methods used to detect them can be found in the Data4Life article on antibodies.
How long does antibody protection last?
There is general agreement among scientists that most people who produce antibodies (immunoglobulin G or IgG) are protected against a second infection. The question is: how long does this protection last? Because we have only known about this particular coronavirus for a short period of time, we still don’t know for sure. Based on studies of previous coronaviruses such as SARS-CoV (identified in 2002) and MERS-CoV (the virus responsible for Middle Eastern Respiratory Syndrome), it was initially assumed that antibody-mediated immunity against the current coronavirus would last for two to three years at least [8]. However, more recent studies published in “Nature Medicine” in the middle of June 2020 suggest that antibodies may only last two to three months [9], especially in people with milder symptoms.
Can other immune cells provide additional protection?
Low antibody levels alone don’t necessarily mean that a re-infection will occur since other factors also seem to play a role in immunity to SARS-CoV-2. For example, studies at Columbia University suggest that, in addition to specific antibodies, a powerful T-cell response to the virus could play a critical role in long-term immunity to SARS-CoV-2 [10]. More recently, researchers at the University of Tübingen came to a similar conclusion. Their studies showed that T cells may have just as important a role as antibody-producing B cells in fighting off the SARS-CoV-2 virus. This immune response is linked to previous exposure to common cold coronaviruses, in other words to cross-immunity [11].
Cross-immunity between SARS-CoV-2 and common cold coronaviruses
Cross-immunity is another factor that needs to be considered when assessing immunity to SARS-CoV-2. Back in May 2020, studies conducted by scientists at University College London suggested that prior exposure to common cold coronaviruses could explain why many people infected with SARS-CoV-2 show little in the way of clinical symptoms or are asymptomatic [12]. In fact, there is more than one type of coronavirus. There are several types, most of which have been around for decades and cause harmless illnesses like the common cold. In other words, people who have previously been infected with other similar, but less dangerous, coronaviruses could produce antibodies that protect them–to some degree at least–against the current SARS-CoV-2 virus. These antibodies could also lead to false-positive results in coronavirus antibody tests [13]. This means that people can test positive for SARS-CoV-2 even though they only have antibodies against other, harmless, coronaviruses.
These sometimes contradictory findings show that the question of immunity to SARS-CoV-2 is a complex and multi-faceted one and that further research is needed to answer it.
3. Immunity certificates
Closely linked with the question of immunity is the issue of immunity certificates (or “immunity passports”) and their potential role in fighting the current coronavirus pandemic.
At an early stage in the current coronavirus pandemic, politicians and scientists opened up a debate about immunity documentation and immunity certificates. These documents would confirm that a person has already had the disease and is immune due to natural infection or, in the future, is immune due to vaccination. Governments in countries such as Chile, Germany, the United Kingdom, Italy, and the United States have debated the concept of immunity certificates at length.
Can immunity certificates prevent future lockdowns?
The idea behind the certificates would be to exempt the increasing proportion of the population that has developed immunity from lockdown restrictions. Especially given the imminent global recession, this approach could provide an opportunity to re-open certain areas of public life and boost the economy without unnecessary risk to the health of the population. However, this is based on the assumption that infection with SARS-CoV-2 results in permanent, or at least long-term, immunity. As discussed above, there is still no clear understanding of when exactly a person can be considered immune and how long this immunity may last.
So for now, the reliability of immunity documentation remains questionable. In the international context in particular, an immunity documentation program of this type would require a common global understanding of SARS-CoV-2 immunity as well as uniform quality control.
Ethical implications of immunity certificates
In addition to the discussions in the medical community, the introduction of immunity certificates has sparked a broader social debate. This debate is focused mainly on the question of whether, and to what extent, immunity certificates could lead to certain groups of people being stigmatized, now or in the future. The German Parliament has taken up this debate and the German Ethics Council is currently grappling with the potential implications. [14,15]
In conclusion, despite the complexity of the immune system and related issues, we can do a lot to improve immunity at both an individual and population level.
This is a pandemic in a digital age and digital solutions can be used to inform the population, monitor symptoms, and slow the progress of the disease.
The contents of this article reflect the current scientific status at the time of publication and were written to the best of our knowledge. Nevertheless, the article does not replace medical advice and diagnosis. If you have any questions, consult your general practitioner.
Originally published on