1. The cornerstones of immunity
1.1 Distinguishing self from nonself
Immunity is the ability of an individual to identify pathogens and render them harmless if necessary. To do this, the immune system needs to be able to distinguish between “self ”and “nonself” [1]. Otherwise, we would be constantly battling our own bodies. The human body is able to recognize potentially harmful substances and structures that originate outside the body. It identifies infectious microbes (bacteria, viruses, fungi, and parasites) as foreign based on chemical structures found on the surfaces of cells. Using similar pattern recognition mechanisms, it can also identify other substances as foreign or harmful, e.g. pollen, dust, and heavy metals as well as toxins produced in the body and diseased cells transformed by mutations. So, the body is capable of discriminating not only between self and nonself, but also between harmful and harmless. It is thought that this ability to detect patterns developed very early in our evolutionary history and that we inherited it from invertebrate ancestors.
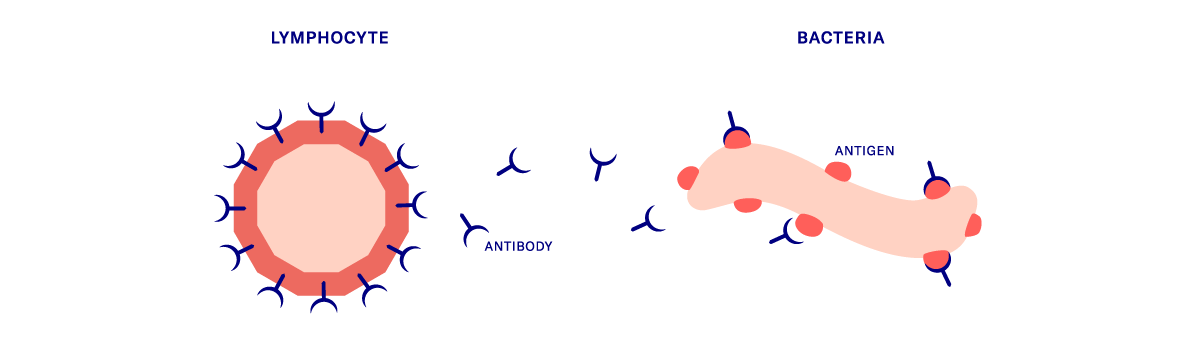
1.2 Immunogens and antigens: what are they?
An immunogen is any substance or microorganism that stimulates an immune response [2]. An immunogen that also causes antibodies to be produced (see antibodies below) is called an antigen [3]. The ability of the body to identify immunogens or antigens as foreign or harmful based on the structures found on their surface is another cornerstone of immune function.
2. Immune function
Our immune defense system rests on two main pillars: the innate (nonspecific) immune system and the acquired (adaptive) immune system. Each of these systems has two components: a cellular component mediated by immune cells and a humoral component mediated by chemical messengers. The term “humoral” comes from the Latin hūmorālis and refers to molecules dissolved in body fluids that support the immune response. The innate immune system responds to general stimuli and can be activated quickly. However, it lacks a memory. The acquired immune system, on the other hand, can remember prior encounters with an antigen. This allows it to mount a highly specific response when it encounters the antigen again. Although it does not react immediately, the acquired immune system can provide long-term or even permanent protection thanks to its ability to remember.
2.1 The innate immune system
The innate immune system is more about speed than specificity and relies first and foremost on physical barriers, physiological secretions, and generalized reactions.
Physical barriers and physiological secretions
Before a pathogen can reach the inside of the body, it has to break through a number of physical barriers. The skin and mucous membranes, cornea, and tiny hair-like structures in the nose act as the first line of defense. If foreign particles manage to overcome these initial hurdles, they then face the hostile acid conditions of our gastric juices, vaginal flora, urine, and skin secretions. Even bacteria are partly responsible for influencing the pH of the local body environment and creating permanently unfavorable conditions for the growth of many pathogens [4].
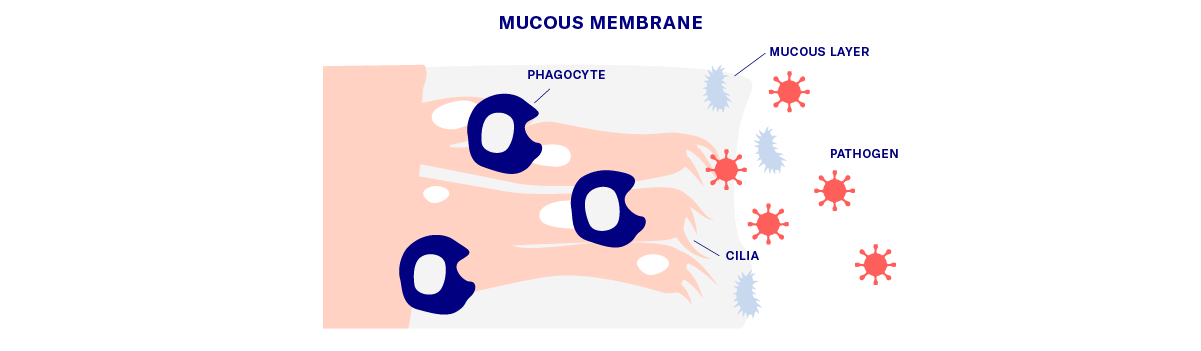
Cellular components and defense mechanisms
If pathogens succeed in overcoming the body’s first line of defense, immune cells and chemical messengers are activated in the next phase. The various types of white blood cells (leukocytes) that circulate in the lymph and blood and monitor all parts of the body are an essential element of the innate immune system. Scavenger cells (phagocytes) engulf pathogens that they identify based on surface markers. They digest the pathogens in a process known as phagocytosis and then present the resulting fragments on receptors on their surface. Cells that present tiny, digested antigen components on their surface in this way are referred to as “antigen-presenting cells” (APCs). The antigen presentation process indicates that a pathogen has invaded the body and activates a series of other defense mechanisms. Infected cells also release chemical messengers into the bloodstream to recruit further immune cells, such as macrophages and mast cells, which are white blood cells that trigger inflammatory reactions.
The complement system
Immune cells are not the only participants in immune defense. As already mentioned, humoral (see explanation above) components also play their part. The complement system (from the Latin complementum, which means “something that fills up or completes”) is an essential component of the humoral immune response. It involves a cascade of chemical reactions in which each messenger activates the next messenger in the pathway. This in turn activates further defense mechanisms, which, for example, efficiently label infected cells for phagocytosis or cause pathogens to clump together so that they are easier to destroy. Complement proteins can also break down the surfaces of pathogens, slowing down their proliferation [4].
This collection of reactions can be likened to an attack mounted on several fronts by a large army.
2.2 The acquired immune system
The acquired immune system is able to generate a tailored immune response by storing previous exposure to antigens in the immunological memory. The cellular constituents of the acquired immune system belong to a subgroup of white blood cells known as lymphocytes and are referred to as B cells and T cells. B cells are named after the bursa of Fabricius, a lymphoid organ of birds in which these cells were first discovered. Each of the millions of B cells produced by the body has unique receptors on its surface that match only one antigen. Incredibly, no two B cells have the same receptors. A naive B cell is a B cell that has not been exposed to an antigen that matches its surface receptor. Once the B cell is exposed to a matching antigen, the surface receptor binds to the antigen based on the lock and key principle [5].
Antibody production
This process causes the naive B cell to mature and differentiate into a memory cell or a plasma cell. Newly formed memory cells have exactly the same surface receptors as the original B cells. Plasma cells also produce the same receptors, but they are not bound to the cell surface. Instead, they are secreted into the lymph and blood, where they are referred to as antibodies. Once they are no longer bound to cells, antibodies represent the humoral component of the acquired immune system.
After encountering an antigen for the first time, the acquired immune system can remember the characteristics of that antigen. If the antigen appears in the body again, the tailored production of specific antibodies can be switched on immediately, which in most cases can prevent illness.
The role of T cells
T cells originate in the bone marrow but migrate to the thymus gland (from which they take their name) before birth and during the first years of life. In the thymus, they are trained to react to foreign antigens while tolerating antigens that are produced in the body (self-tolerance). Unlike antibodies, T cells cannot bind directly to antigens. Instead, T-cell receptors (TCRs) on their surface bind the antigens that are presented by antigen-presenting cells (APCs, see above) [6]. Since most APCs are primarily associated with the innate immune system, T cells act as a bridge between the innate and acquired immune responses.
There are different types of T cells, each with a different role in the immune response, e.g. helping B cells to secrete antibodies or eliminating infected cells [6].
The entire system functions as a sophisticated network of interconnected and interdependent cellular and humoral components that ensures lasting protection against potential harm.
3. Immunodeficiencies: when the system doesn't work
An intact immune system cannot be taken for granted. Both congenital and acquired defects of the immune system can impair our resistance to pathogens. Primary immunodeficiencies are present at birth or develop in early childhood. They are rare and often hereditary. Acquired immunodeficiencies are caused by a variety of factors, ranging from malnutrition, exposure to harmful substances, cancer, or organ transplantation to medication side-effects, hormonal imbalances, or autoimmune diseases [7].
4. Boosting the immune system with home remedies and diet
When it comes to boosting the immune system, traditional wisdom and myths abound. There is also a wealth of information available online on the subject. We know that a healthy diet and regular exercise contribute to a healthy immune system, but to what extent has the effectiveness of home remedies actually been demonstrated? Studies have shown that vitamin C deficiency results in impaired immunity and higher susceptibility to infection [8]. Therefore, vitamin C supplementation may be advisable to prevent and treat systemic infections. Whether the same can be said for vitamin D is still unclear. It is suspected that vitamin D deficiency may play a role in the severity of certain chronic inflammatory conditions, however the evidence for taking a vitamin D supplement is inconclusive [9].
The role of the gut flora
The gut flora is made up of the microorganisms that normally live in our digestive tract. The role of a diverse and balanced gut flora in defending the body against disease is the subject of much debate. Indeed, studies have suggested that probiotics (live bacteria in supplement form) could support immune function in the gut. On the other hand, a healthy gut flora seems to depend on a highly personalized balance of bacteria, which is why commercially available probiotics are unlikely to address an individual’s specific needs [10].
Overall, the results of studies investigating the use of home remedies have been variable or inconsistent. To obtain maximum benefit, non-prescription home remedies should always be considered in a highly personalized context.
5. The future is digital
Immunity is a highly complex and multidimensional phenomenon. Its finer points are easier to understand if we consider the pillars on which it is based and the different pathways in the immune system. It is clear that the immune system has its limits and sometimes requires additional support. While we eagerly search for new diagnostic and treatment methods, digital approaches offer forward-looking and readily available solutions. These include relevant apps for personalized monitoring of disease progression and digitalized vaccination systems.
Part 2 of Data4Life’s series of articles on immunity is dedicated to vaccinations, immunity, and proof of immunization in the context of the Coronavirus SARS-CoV-2 pandemic. We also address the potential pioneering role of digital technologies in helping to detect disease and promote public health in the years to come.
The contents of this article reflect the current scientific status at the time of publication and were written to the best of our knowledge. Nevertheless, the article does not replace medical advice and diagnosis. If you have any questions, consult your general practitioner.
Originally published on